Chronic prostatitis – inflammatory disease of the prostate of various etiologies (including non-infectious), manifested by pain or discomfort in the pelvic area and urinary tract problems for 3 months or longer.
I. Introductory part
Protocol name: Inflammatory diseases of the prostate
Protocol code:
ICD-10 code(s):
N41. 0 Acute prostatitis
N41. 1 Chronic prostatitis
N41. 2 prostate abscess
N41. 3 Prostatocystitis
N41. 8 Other inflammatory diseases of the prostate
N41. 9 Inflammatory disease of the prostate, unspecified
N42. 0 prostate stones
Prostate stone
N42. 1 Congestion and bleeding in the prostate
N42. 2 prostate atrophy
N42. 8 Other specified diseases of the prostate
N42. 9 Disease of the prostate, unspecified
Abbreviations used in the protocol:
ALT – Alanine aminotransferase
AST – Aspartate aminotransferase
HIV – Human immunodeficiency virus
ELISA – enzyme immunoassay
CT – Computed Tomography
MRI – magnetic resonance imaging
MSCT – multi-slice computed tomography
DRE – digital rectal exam
PSA – Prostate Specific Antigen
DRE – digital rectal exam
PC - prostate cancer
CPPS – chronic pelvic pain syndrome
TUR – transurethral resection of the prostate
Ultrasound – Ultrasound examination
ED – erectile dysfunction
ECG – electrocardiography
IPSS – International Prostate Symptom Score (international symptom index for prostate diseases)
NYHA – New York Heart Association
Date of development of the protocol: 2014
Patient category: Men of childbearing age.
Protocol user: Andrologists, urologists, surgeons, therapists, general practitioners.
Levels of evidence
level |
Type of evidence |
| 1a | The evidence comes from a meta-analysis of randomized trials |
| 1b | Findings from at least one randomized trial |
| 2a | Findings from at least one well-designed, controlled, non-randomized trial |
| 2b | Evidence from at least one well-designed, controlled, quasi-experimental study |
| 3 | Findings from well-designed non-experimental research (comparative research, correlational research, analysis of scientific reports) |
| 4 | The evidence is based on expert opinions or experiences |
Grades of recommendation
| A | The results are based on homogeneous, high-quality, problem-specific clinical studies with at least one randomized trial |
| IN | Results from well-designed, non-randomized clinical trials |
| WITH | No clinical studies of sufficient quality have been conducted |
classification
Clinical classification
Classification of Prostatitis (National Institute of Health (NYHA, USA, 1995)
Category I – acute bacterial prostatitis;
Category II – chronic bacterial prostatitis, which occurs in 5-10% of cases; Category III – chronic abacterial prostatitis/chronic pelvic pain syndrome, diagnosed in 90% of cases;
Subcategory III A – chronic pelvic inflammatory pain syndrome with an increase in leukocytes in prostatic secretion (more than 60% of the total number of cases); Subcategory III B – CPPS – chronic non-inflammatory pelvic pain syndrome (without an increase in leukocytes in the prostatic secretion (approx. 30%));
Category IV – asymptomatic inflammation of the prostate, detected during examination for other diseases, based on the results of the analysis of prostate secretions or their biopsy (histological prostatitis);
diagnosis
II. Methods, approaches and procedures for diagnosis and treatment
List of basic and additional diagnostic measures
Basic (mandatory) diagnostic examinations carried out on an outpatient basis:
- Collection of complaints, medical history;
- digital rectal examination;
- Completing the IPSS questionnaire;
- Ultrasound examination of the prostate;
- prostate secretion;
Additional outpatient diagnostic examinations: prostate secretion;
The minimum list of examinations that must be carried out when referring to a planned hospitalization:
- general blood test;
- general urinalysis;
- biochemical blood test (determination of blood sugar, bilirubin and fractions, AST, ALT, thymol test, creatinine, urea, alkaline phosphatase, blood amylase);
- microreaction;
- coagulogram;
- HIV;
- ELISA for viral hepatitis;
- fluorography;
- ECG;
- Blood type.
Basic (mandatory) diagnostic examinations carried out at the hospital level:
- PPE (total, free);
- bacteriological culture of prostate secretion obtained after massage;
- transrectal ultrasound examination of the prostate;
- Bacteriological culture of prostate secretion obtained after massage.
Additional diagnostic examinations at hospital level:
- uroflowmetry;
- cystotonometry;
- MSCT or MRI;
- Urethrocystoscopy.
(Evidence level – I, recommendation strength – A)
Diagnostic measures in the emergency stage: not carried out.
Diagnostic criteria
Complaints and anamnesis:
Complaints:
- Pain or discomfort in the pelvic area that lasts 3 months or longer;
- A common location of pain is the perineum;
- a feeling of discomfort may occur in the suprapubic area;
- discomfort in the groin and pelvis;
- discomfort in the scrotum;
- discomfort in the rectum;
- discomfort in the lumbosacral area;
- Pain during and after ejaculation.
Medical history:
- sexual dysfunction;
- suppression of libido;
- Deterioration in the quality of spontaneous and/or sufficient erections;
- premature ejaculation;
- in the later stages of the disease, ejaculation occurs slowly;
- "Eradication" of the emotional coloring of the orgasm.
The impact of chronic prostatitis on quality of life is comparable to the impact of myocardial infarction, angina, and Crohn's disease, according to the Unified Quality of Life Rating Scale (Evidence level - II, recommendation strength - B).
Physical examination:
- swelling and tenderness of the prostate;
- Enlargement and smoothing of the middle groove of the prostate.
Laboratory research
To increase the reliability of the results of laboratory tests, they should be carried out before the appointment or 2 weeks after the end of taking antibacterial agents.
Microscopic examination of prostate secretion:
- Determination of leukocyte count;
- Determination of the amount of lecithin grains;
- Determination of the number of amyloid bodies;
- Determination of the number of Trousseau-Lallemand bodies;
- Determination of the number of macrophages.
Bacteriological examination of prostate secretions: determination of the type of disease (bacterial or abacterial prostatitis).
Criteria for bacterial prostatitis:
- the third portion of urine or prostatic secretion contains bacteria of the same strain at a titer of 103 CFU/ml or more, provided the second portion of urine is sterile;
- a tenfold or greater increase in bacterial titer in the third part of urine or prostatic secretion compared to the second part;
- The third part of the urine or prostatic secretion contains more than 103 CFU/ml true uropathogenic bacteria, which are different from other bacteria in the second part of the urine.
The predominant importance of gram-negative microorganisms from the family Enterobacteriaceae (E. coli, Klebsiella spp. , Proteus spp. , Enterobacter spp. etc. ) and Pseudomonas spp. as well as Enerococcus faecalis in the occurrence of chronic bacterial prostatitis has been proven.
Blood sampling to determine the serum PSA concentration should take place at least 10 days after the DRE. Prostatitis can lead to an increase in PSA levels. However, if the PSA value is above 4 ng/ml, the use of additional diagnostic methods, including a prostate biopsy, is indicated to rule out prostate cancer.
Instrumental studies:
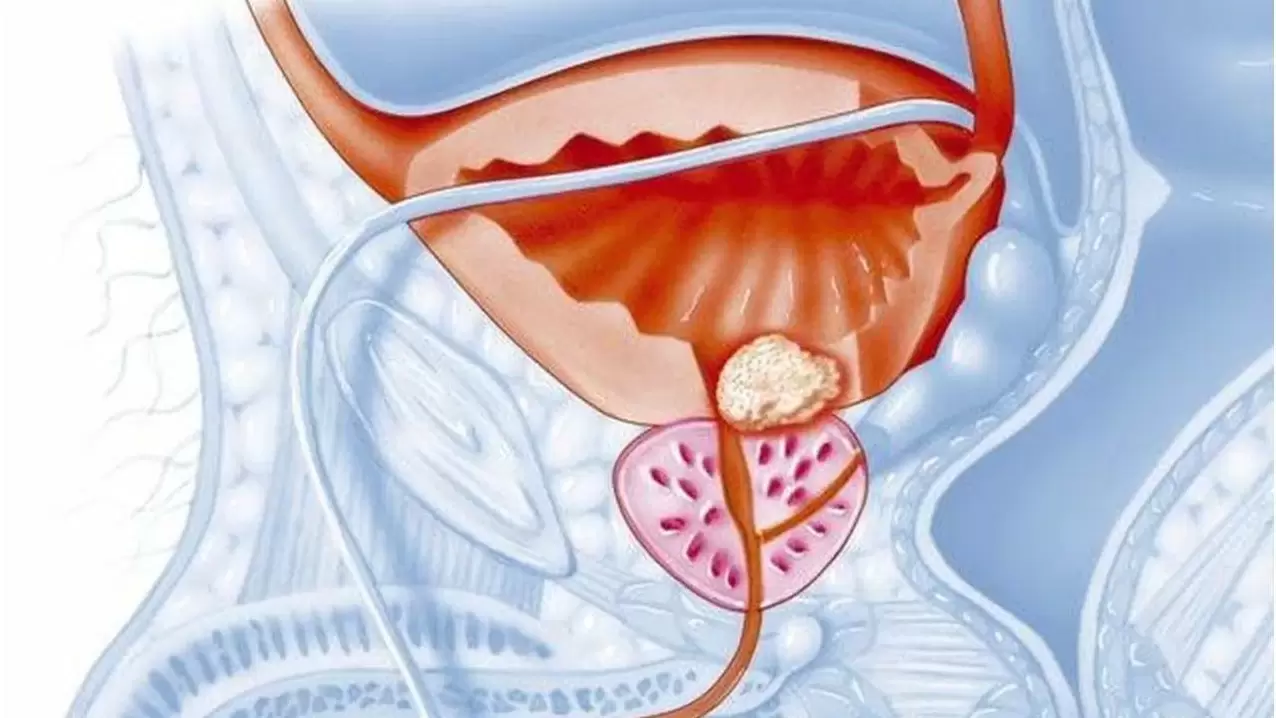
Transrectal ultrasound of the prostate: for differential diagnosis, determining the form and stage of the disease with subsequent monitoring throughout the entire period of treatment.
Ultrasound: assessment of the size and volume of the prostate, echostructure (cysts, stones, fibrous-sclerotic changes in the organ, prostate abscesses). Hypoechoic areas in the peripheral zone of the prostate are suspicious for prostate cancer.
X-ray examinations: if a bladder outlet obstruction has been diagnosed, to clarify the cause and determine further treatment tactics.
Endoscopic methods (urethroscopy, cystoscopy): are performed according to strict indications for the purpose of differential diagnosis and are covered with broad-spectrum antibiotics.
Urodynamic studies (uroflowmetry): determination of the urethral pressure profile, pressure/flow study,
Cystometry and myography of the pelvic floor muscles: in suspected bladder outlet obstruction, which is often accompanied by chronic prostatitis, as well as neurogenic disorders of urination and the function of the pelvic floor muscles.
MSCT and MRI of the pelvic organs: for differential diagnosis of prostate cancer.
Advice on consulting specialists: Consult an oncologist - if the PSA value is more than 4 ng/ml to rule out malignant prostate formation.
Differential diagnosis
Differential diagnosis of chronic prostatitis
For differential diagnosis, the condition of the rectum and surrounding tissues should be assessed (Evidence level – I, recommendation strength – A).
Nosologies |
Characteristic syndromes/symptoms | Differentiation test |
| Chronic prostatitis | The average age of the patients is 43 years. Pain or discomfort in the pelvic area that lasts 3 months or longer. The most common location of pain is the perineum, but discomfort can also occur in the suprapubic, inguinal area of the pelvis, as well as in the scrotum, rectum, and lumbosacral region. Pain during and after ejaculation. Urinary dysfunction often manifests itself in symptoms of irritation, less commonly in symptoms of bladder outlet obstruction. |
DURING - You may notice swelling and tenderness of the prostate gland and sometimes enlargement and smoothness of the medial groove. For differential diagnosis, the condition of the rectum and surrounding tissues should be assessed. Prostatic secretion – Determine the number of leukocytes, lecithin grains, amyloid bodies, Trousseau-Lallemand bodies and macrophages. A bacteriological examination of prostatic secretion or urine obtained after a massage. Based on the results of these studies, the type of disease is determined (bacterial or abacterial prostatitis). Criteria for bacterial prostatitis
Ultrasound of the prostate in chronic prostatitis has high sensitivity but low specificity. The study allows not only to carry out differential diagnosis, but also to determine the form and stage of the disease with subsequent monitoring throughout the entire course of treatment. Ultrasound allows assessment of the size and volume of the prostate as well as the echo structure |
| Benign prostatic hyperplasia (prostate adenoma) | It is more commonly seen in people over 50 years old. A gradual increase in urination and a slow increase in urinary retention. An increased frequency of urination at night is typical (in chronic prostatitis, increased frequency of urination during the day or early in the morning). | PRI – the prostate is painless, enlarged, densely elastic, the central furrow is smoothed, the surface is smooth. Prostatic secretion – the amount of secretion increases, but the number of leukocytes and lecithin grains remains within the physiological norm. The secretion reaction is neutral or slightly alkaline. Ultrasound - deformation of the bladder neck is observed. The adenoma protrudes into the bladder cavity in the form of bright red, lumpy structures. There is a significant proliferation of gland cells in the cranial part of the prostate. The structure of the adenomas is homogeneous with regularly shaped areas of darkening. The gland enlarges in the anteroposterior direction. In fibroadenoma, bright echoes from the connective tissue are detected. |
| Prostate cancer | People over 45 years of age are affected. When diagnosing chronic prostatitis and prostate cancer, the localization of pain is identical. Pain in prostate cancer in the lumbar region, sacrum, perineum and lower abdomen can be caused both by a process in the gland itself and by metastases in the bones. Rapid development of complete urinary retention often occurs. Severe bone pain and weight loss may occur. | IF - individual cartilage density nodules or lumpy dense infiltrations of the entire prostate are noted, which are limited or spread to surrounding tissues. The prostate is motionless and painless. PSA – more than 4. 0 ng/ml Prostate biopsy – a collection of malignant cells in the form of duct casts is determined. Atypical cells are characterized by hyperchromatism, polymorphism, variability in size and shape of nuclei, and mitotic figures. Cystoscopy – pale pink lumpy masses are noted surrounding the bladder neck in a ring (the result of infiltration of the bladder wall). Often swelling, hyperemia of the mucous membrane, malignant proliferation of epithelial cells. Ultrasound - asymmetry and enlargement of the prostate, its significant deformation. |
Treatment
Treatment goals:
- Elimination of inflammation in the prostate;
- Relieving symptoms of exacerbation (pain, discomfort, impaired urination and sexual function);
- Prevention and treatment of complications.
Treatment tactics
Non-drug treatment:
Diet number 15.
Mode: General.
Drug treatment
In the treatment of chronic prostatitis, it is necessary to use several drugs and methods at the same time that act on different parts of the pathogenesis and ensure the elimination of the infectious agent, the normalization of blood circulation in the prostate and adequate drainage of the prostatic acini, especially in the peripheral zonesthe level of essential hormones and immune reactions. Antibacterial drugs, anticholinergics, immunomodulators, NSAIDs, angioprotectors, vasodilators, prostate massage are recommended, and therapy with alpha blockers is also possible.
Other treatments
Further outpatient treatments:
- transrectal microwave hyperthermia;
- Physiotherapy (laser therapy, mud therapy, phonoelectrophoresis).
Other types of services at the inpatient level:
- transrectal microwave hyperthermia;
- Physiotherapy (laser therapy, mud therapy, phonoelectrophoresis).
Other types of treatment in the emergency stage: not provided.
Surgical intervention
Surgical procedures performed on an outpatient basis: not performed.
Surgical intervention in the inpatient area
Types:
Transurethral incision at 5, 7 and 12 o'clock.
Notes:
Performed in hospital if the patient suffers from prostatic fibrosis with the clinical picture of bladder outlet obstruction.
Types:
Transurethral resection
Notes:
Use in calcific prostatitis (especially localized stones that cannot be treated conservatively in the central, transient and periurethral areas).
Types:
Resection of the seminiferous tubercle.
Notes:
with sclerosis of the seminal tubercle, accompanied by occlusion of the ejaculatory and excretory ducts of the prostate.
Preventive measures:
- give up bad habits;
- Elimination of the influence of harmful influences (cold, physical inactivity, prolonged sexual abstinence, etc. );
- Diet;
- spa treatment;
- Normalization of sex life.
Additional management:
- observation by a urologist 4 times a year;
- Ultrasound of the prostate and residual urine in the bladder, DRE, IPSS, prostate secretion 4 times a year
Indicators of treatment effectiveness and safety of the diagnostic and treatment methods described in the protocol:
- Absence or reduction of characteristic complaints (pain or discomfort in the pelvis, perineum, suprapubic area, pelvic inguinal area, scrotum, rectum);
- Reduction or absence of swelling and tenderness of the prostate according to the results of DRE;
- Reducing inflammatory indicators of prostate secretion;
- Reducing the swelling and size of the prostate according to ultrasound.
























